Medicaid Unwinding
During the COVID-19 Pandemic, protections were put in place so that Medicaid recipients kept coverage even if they no longer qualified. This was done so people had access to COVID-19 testing and treatment.
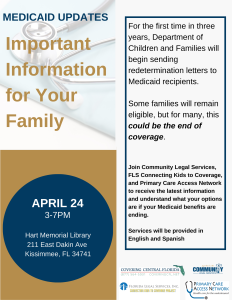
These special protections are coming to an end, and the Department of Children and Families (DCF) has begun sending out redetermination letters for the first time in 3 years.
Some families will remain eligible, while others will not.
If you receive a redetermination notice and need assistance, contact CLS. Visit our page on Medicaid for more information about eligibility.
WHAT ARE YOUR RIGHTS?
As the Medicaid COVID-19 protections begin to unwind, each state has created a redetermination plan describing how they will review the eligibility of all Medicaid recipients by Summer 2024. Florida’s Redetermination plan can be found here.
As part of the plan:
- The Department of Children and Families (DCF) will review eligibility for all Medicaid recipients between March 2023 and April 2024.
- Terminations will begin April 30, 2023.
- DCF will do an “ex parte” review, using the information they have available to review eligibility before requesting additional information.
- All new applications will be processed under pre-pandemic rules.
DCF will do an “ex parte” review to determine eligibility. This means they will use the information they have available to review eligibility before reaching out to recipients for more information. DCF will use information submitted as part of applications for other benefits like SNAP and TANF and other sources such as wage information from the State Wage and Income Collection Agency (SWICA) to do this review.
As part of this review, if you are no longer eligible for coverage in your current coverage group, DCF must determine if you are eligible for coverage in one of the other Medicaid categories, including the medically needy program and Florida KidCare.
If DCF has enough information to approve your renewal, they will send an approval notice with no action required by you.
If there is not enough information for DCF to approve you, they will send a notice 45 days before Medicaid benefits are scheduled to end with instructions on how to complete the redetermination process.
DCF is required to provide notice, in language you can understand, if they approve, deny, terminate, reduce, or suspend Medicaid benefits.
If DCF has enough information to approve your renewal, they will send an approval notice with no action required by you.
If DCF is unable to approve after reviewing the information they, they must send a redetermination notice 45 days before Medicaid benefits are scheduled to end with instructions on how to complete the redetermination process.
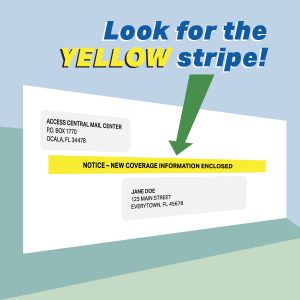
Notices regarding Medicaid redetermination will come in a yellow striped envelope.
If you do not complete the redetermination process, DCF must send an “adverse action notice” at least 10 days before benefits end. In this notice DCF must explain the reason for the termination, the date benefits will end, and appeal rights, including how to request a Fair Hearing.
While all Medicaid recipients will have their eligibility reviewed, some groups are more likely to lose Medicaid coverage than others. The groups most at risk of losing Medicaid coverage are:
- Households whose income has increased
- Parents and caretaker relatives whose youngest child turned 18
- Women who began receiving Medicaid when pregnant
- Children who have moved into a new age group
- Those who met their “share of cost” under the medically needy program
Many individuals in these categories are no longer eligible for Medicaid and will lose benefits when their redetermination occurs.
If you or a family member are at risk of losing Medicaid, there are other options available to you.
WHAT DO YOU NEED TO DO?
If you or a member of your household have Medicaid, update your information with DCF now. You can do this by logging onto your myACCESS account online and clicking the “Report Changes” button.
You can also update your contact information using DCF’s virtual assistant by clicking on the icon when you visit DCF’s Medicaid information page.
If you are unable to update your contact information online, call DCF at 850-300-4DCF (4323).
By signing up for email or text message notifications, you can receive electronic reminders when it is time for your redetermination.
Logon to your myACCESS account online to opt-in to receive notice by email or text message. You will receive an email when you have a notice ready to view in your account.
You can log on to your myACCESS account online now to check your redetermination date. This will give you time before a DCF notice is sent out to determine what steps you might have to take.
Notices regarding Medicaid redetermination will come in a yellow striped envelope like this image provided from DCF:
If you receive a notice requesting more information, you must respond before the deadline otherwise, DCF will terminate benefits.
If you receive a notice and need help understanding what to do, contact us.
If you have received an adverse action notice stating that your Medicaid benefits will be terminated, you have 90 days from the date of the notice to ask for a Fair Hearing. A Fair Hearing is the process that allows you to dispute the termination decision if you believe it was decided unfairly. Instructions on how to ask for a Fair Hearing should be included with the notice of termination that DCF sends.
You have only 10 days to ask for a Fair Hearing in order to keep your Medicaid benefits pending the outcome of your appeal.
If you know you are no longer eligible for Medicaid, do not ask for a Fair Hearing. Medicaid has strict eligibility requirements that DCF must follow. Requesting a Fair Hearing when you know you are no longer eligible will only cause further delays for DCF as they work to review eligibility for all current recipients.
For a review of your eligibility and to determine if filing an appeal is right for you, contact us.
For those who are no longer eligible for Medicaid, there are other options available. Click the links for more information.
- Florida KidCare refers to a group of healthcare programs available to children up to age 18: Medicaid, MediKids, Florida Healthy Kids, and the Children’s Medical Services (CMS) Health Plan. There are free, subsidized and full-pay options based on family income and household size. Most families pay nothing for these programs, and many pay as little as just $15 or $20 a month.
- Medically Needy Program is for those who would qualify for Medicaid except that their income is too high. Those enrolled in this program must provide DCF with proof they have met a monthly share of cost (similar to an insurance deductible) before Medicaid is active for the month.
- Medicare is a federal health insurance program for those who are age 65 or older, and some younger people who are disabled.
- Those who qualify for disability benefits through Social Security automatically qualify for health benefits – Medicaid or Medicare depending on their situation. If you are an adult who has a health condition that prevents you from working or have a child who has a health condition that seriously limits their daily activities you can find more information about applying here. See our Social Security Benefits page for more information about the different programs and eligibility requirements.
- Commercial coverage – ie: insurance through an employer
- Health Insurance Marketplace(Obamacare) Federally Subsidized Health Programs – The Healthcare Marketplace offers insurance enrollment options and can tell you if you qualify for premium tax credits and other savings that can make coverage more affordable. Find a list of Federally-Certified Navigators who can help you review your options and choose a plan that is right for you and your family here. Federally Qualified Health Centers provide primary care services on a sliding fee scale based on your ability to pay. These clinics can also accept Medicaid and Medicare. You can find a clinic locator here.
- Free and Charitable Clinics provide free or low-cost health care services to the uninsured and underinsured. You can find a clinic here..
- Mental health resources
- Prescription drug assistance – Many prescription drug makers have programs that provide free or reduced cost medications. You must contact the maker of your prescription to see if they have a program like this. There are several other programs including FloridaRxCard, the Florida Discount Drug Card Program, and GoodRx that can help you find discounts on medications.
WHAT TO CONSIDER BEFORE TAKING ACTION?
For more information about eligibility visit:
Usually you can only enroll in Medicare or Federally Subsidized Health Programs through the Healthcare Marketplace (Obamacare) during the annual enrollment period unless you meet the requirements for a special enrollment period (SEP). Both Medicare and the Healthcare Marketplace are offering special enrollment periods to those who lose Medicaid coverage as part of the unwinding of the COVID-19 protections.
Medicare special enrollment period
- Applies to those who receive a notice after January 1, 2023 of a future termination of Medicaid benefits.
- The SEP starts for the person when they receive notice of future termination and ends 6 months after their termination.
- Under this SEP, you can choose a Medicare effective date that is either the month after the application or retroactive to the date of the termination. If you choose retroactive coverage, you will be responsible for the premiums owed for that time.
- A person who qualifies for this SEP can avoid late enrollment penalties.
Healthcare Marketplace special enrollment period
- Applies to those who attest Medicaid or CHIP will be terminated between March 31, 2023 and July 31, 2024.
- Have to apply or update an existing application at HealthCare.gov between March 31, 2023 and July 31, 2024.
- There are 60 days to pick a plan after applying or updating an existing application. Coverage will start the month after the plan is selected.
- Can apply or update an existing application under this SEP up to 60 days before the date Medicaid termination will take place. This helps to prevent a gap in coverage.
- See this FAQ from the Center for Medicare and Medicaid Services (CMS) for more information.
Avoid long Call Center wait times by using the virtual assistant on DCF’s website or by logging into your myACCESS account online to make updates and get information, when possible. Through your account you can access notices, upload requested documents, update your information, and check your redetermination date.
If you currently have Medicaid, do not file a renewal or new application before it is your time for redetermination.
If you know you are no longer eligible for Medicaid, do not file a renewal or new application.
Filing an application before your redetermination date or when you know you are no longer eligible will only cause further delays for DCF as they work to review eligibility for all current recipients.
Remember, DCF is using the information they have to review eligibility first. Not all recipients will have to provide additional information or file a new application to receive an approval.
DCF will send a notice at least 45 days before your redetermination date if they need information from you, including a new application or renewal.

 Home
Home